Anaesthesia with surgical precision
Ultrasound technology will soon be helping doctors to anaesthetise patients more accurately. And the technology is being developed in Trondheim.
Ultrasound is being used in an increasing number of medical contexts, including diagnostics, treatment and examinations. Imaging techniques are also being used during narcosis in a process called ‘ultrasound-guided regional anaesthesia’, during which a greater part of the patient’s body is anaesthetised prior to an operation. This involves a doctor injecting the anaesthetic directly around the key nerves in question.
Ultrasound-guided regional anaesthesia is a preferred approach in many cases because it can spare the patient unnecessary narcosis, and ensures that the anaesthetic is applied correctly and the subsequent operation carried out with the least possible pain and discomfort to the patient. If this also results in shorter hospital stays, then society as a whole also benefits.
Assisting interpretation
However, the technique requires a high degree of accuracy. For this reason, researchers at SINTEF are currently developing software that can assist doctors in interpreting ultrasound images in real time with the help of 3D images – in this case involving regional anaesthesia of the main nerve running through the thigh. The aim here is to achieve precision within a few millimetres of the target.
SINTEF researcher Frank Lindseth emphasises that this tool is intended to act as an assistant and a guide during the ultrasound-guided insertion of the needle. It is not a robot.
In order to understand ultrasound images, they must be closely examined and interpreted, and this is a very demanding task requiring detailed knowledge and experience. And it doesn’t suit everyone. Many doctors attempt to learn the procedure, but never get as far as performing an injection because they encounter major problems in interpreting the ultrasound images. Moreover, interpretations vary even among experts, in spite of their many years of experience.
The ultrasound reference model
Thus the work that Lindseth and his team have carried out has included generating a reference model describing how images of the human body should be interpreted based on the somewhat cryptic ultrasound images. This has been carried out in close collaboration with doctors at St. Olav’s University Hospital in Trondheim.
Kai F. Johansen is a Senior Consultant at the Orthopaedic Unit at St. Olav’s and has been a key figure in the development of the SINTEF software. He will soon be testing the assistant at the hospital.
His work has involved locating and tracing the body’s so-called ‘anatomical landmarks’ – that is to say key structures within the body as displayed on the ultrasound images during anaesthesia.
An excellent aid
“The challenge doctors face when interpreting ultrasound images is finding what they’re looking for”, says Lindseth. “Their task is to navigate on the basis of known anatomical landmarks within the body – in this case to locate the right nerve so that they can accurately position the needle. This applies both to anaesthesia and pain relief procedures. Our findings show that even among the experts there is a great deal of variation when it comes to interpreting the ultrasound images and accurately locating structures within the body”, he says.
Johansen believes that an ultrasound guide such as this will become an excellent aid to doctors.
“The assistant will be very useful for training doctors in the interpretation of ultrasound images”, he says. “Anatomical landmarks such as blood vessels and membranes are key aids in identifying ultrasound-guided nerve blocks. If you can spot these on the ultrasound images, it becomes easier to localise the nerve that has to be anaesthetised”, explains Johansen.
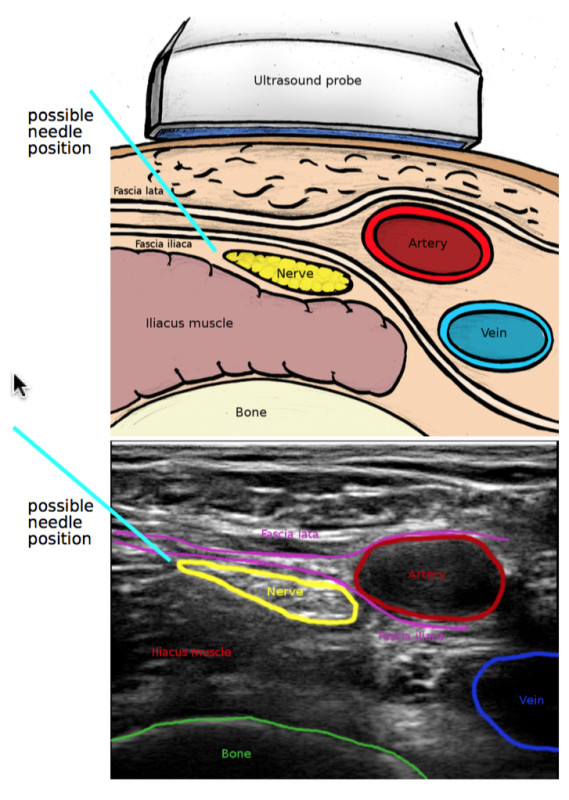
Locating and tracing: A cross-section of the anatomy of the groin, and identification of the so-called anatomical landmarks. The ultrasound image: The assistant tags the key anatomical landmarks within the body. Same section as in the figure. Illustration: Helene E. Mørk.
“One particular challenge has been the variation in the interpretations made by experts”, he says. “This makes it more difficult to establish a reference model to which the assistant can attempt to find matches. This also says something about the level of difficulty involved in developing a robust, entirely automatic and real time system”, adds Lindseth.
3D-guided injection
By using the reference model as a template, the team has developed a software programme that will be installed in ultrasound machines to act as a guide and assistant during the use of ultrasound on patients. A sensor in the ultrasound probe communicates its position using the programme, which then displays 3D images of key anatomical landmarks, and subsequently interprets what it is being revealed by the ultrasound signals. Furthermore, it will be possible to follow the progress of the needle to precisely the location where the injection is required.
The entire process is complicated by the fact that humans refuse to be standardised. We are all different, and some of us are more different than others.
“There can be enormous anatomical differences from patient to patient”, says Lindseth. “So it isn’t difficult to imagine that this is a challenging project”, he says.
This is the team behind the new technology: Janne Beate Bakeng, Erik Smistad, Daniel Høyer Iversan, Kaj F. Johansen, and Frank Lindseth. Photo: Kathinka Høyden.
Ever-increasing need
“Sooner or later, the need for this type of assistant will begin to increase”, explains Lindseth. “Knowledge and experience linked to the interpretation of ultrasound images will be in ever-greater demand once ultrasound is applied in an increasing number of new procedures. Our task is to develop this into a user-friendly tool”, he says.
There are many different regional anaesthesia procedures, and all of them require an ultrasound assistant. If SINTEF’s system is well received, the development of assistants for the remaining procedures will also become a hot topic.
Early next year, the programme will be the subject of clinical tests carried out by experts in the Netherlands, Ireland and Germany.
The project is funded by the EU, and SINTEF is working together with organisations in several European countries, including Germany, France, Greece, Spain, Sweden and the UK.