New technique yields healthier blood vessels after heart surgery
Surgeons often take a blood vessel from your leg to graft onto your heart during a coronary bypass surgery. The practice can lead to scarring in many patients, which in turn can cause another heart attack. A new technique under development may help prevent this problem.
In coronary bypass surgery, a vein from the leg is often grafted around problematic blocked vessels near the heart. However, this technique often leads to formation of scar tissue, which can cause further blockages and lead to another heart attack. A new technique developed by NTNU researchers for extracting the blood vessel from the leg shows a reduction in problematic scar tissue growth.
Heart attacks and angina occur when the vessels that supply the heart with blood become clogged with plaque. In some cases, this blockage can’t be removed, and coronary bypass surgery is the solution.
Coronary bypass involves taking a healthy vein from elsewhere in the body, most commonly one of the large veins from the inside of the leg, and sewing it in around the blocked vessel. This is called a graft.
However, there is a risk that the graft becomes blocked as well, the main cause of this being scarring caused by damage to the innermost layer of the artery wall (intimal hyperplasia).
Less scarring with new technique
Usually, surgeons only take the vein from the patient’s leg. But now, NTNU researchers are studying the effect of a new method that involves harvesting some of the tissue around the vein as well. The idea is that this will prevent damage to the vein walls during the transplant.
“Six months after surgery, scar tissue formation around the graft was clearly lower in patients who had been treated using the new transplant technique,” says PhD candidate Øystein Pettersen at NTNU’s Department of Circulation and Medical Imaging. He is also a doctor in specialization at the thoracic surgery clinic at St. Olavs Hospital in Trondheim.
Pettersen is the first author of an article published in the Journal of the American College of Cardiology.
Advanced measurement method
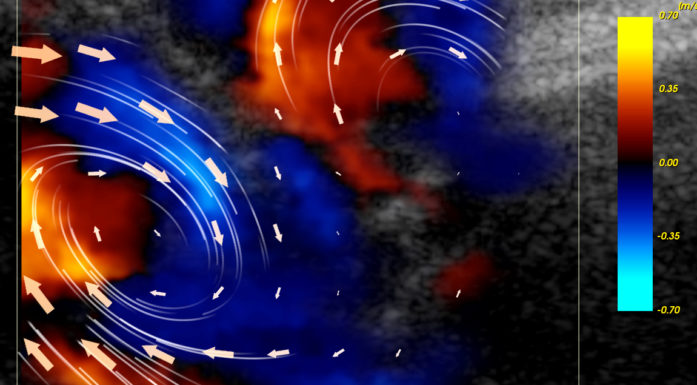
Patients involved in the study were randomly assigned to one of the two treatment methods. The amount of scarring six months after surgery was measured using a highly advanced imaging method called optical coherence tomography (OCT). OCT uses infrared light to create very high resolution images, which in this case allows researchers to precisely measure the thickness of the innermost layer of the artery wall, called the intima.
“The thickness of the intima was on average 0.36 millimeters in patients who had received conventional treatment. In the group where the new technique for vein harvesting was used, the graft was significantly less constricted, with an average thickness of 0.27 millimeters,” explains Pettersen. “There was also less variation in the vein wall thickness in the group where the new method was used.”
Five years of follow-up
The researchers could not, however, show any significant difference in the number of vein grafts that were completely blocked in the two groups, which totalled six from the conventional treatment method and four from the new technique.
“We can’t expect to see a difference with such a short follow-up period. But it will be very interesting to continue following these patients,” Pettersen concludes.
Patients in the study underwent surgery at St. Olavs Hospital between April 2013 and December 2014. A total of 100 patients participated, and the researchers plan to do further studies to follow up on the effects of their technique for the next five years.
Reference: Øystein Pettersen, Rune Wiseth, Knut Hegbom, Dag Ole Nordhaug. Pedicled Vein Grafts in Coronary Surgery Exhibit Reduced Intimal Hyperplasia at 6 Months. Journal of the American College of Cardiology, Volume 68, Issue 4, 26 July 2016, Pages 427-429