Botox blocks out facial pain
Patients with chronic facial pain get their teeth pulled, take a bunch of painkillers and are on a perpetual trek between health services – without finding anything that works to ease the pain. An NTNU researcher thinks Botox can help.
NTNU PhD candidate Kent Are Jamtøy is pursuing innovative medicine. No one has previously tried what he is testing on 30 patients. His research is based on using a high-precision Multiguide surgical instrument to inject Botox and temporarily paralyze the sphenopalatin ganglion nerve deep in the face, behind the sinuses and near the brain.
Turns off the alarm
“We believe that for some reason the ganglion has run riot and sends signals to the brain that are interpreted as pain. By using Botox to turn off the pain signals for a spell, we want to get the brain out of alarm mode,” says Jamtøy.

The research being done by PhD candidate Kent Are Jamtøy may be important in helping people with certain types of facial pain and headaches. Photo: Svein-Inge Meland
As he explains, “once the alarm has been turned off, we think the brain will handle the nerve signals normally as they return and the Botox wears off. The hypothesis is that sensitivity decreases and the patient’s quality of life improves dramatically.”
The study is part of Jamtøy’s PhD work at NTNU’s Department of Neuromedicine and Movement Science.
- You may also like: One-quarter of Norwegian teens have migraines
Promising results
Although the trial is experimental, the researcher is not just taking a stab in the dark.
The Multiguide instrument being used to navigate in the body and inject the Botox was developed at NTNU. Numerous safety studies have been carried out at St. Olav’s Hospital in connection with the approval process for Multiguide. These studies have shown very promising results when injecting Botox into the sphenopalatin ganglion nerve for severe headaches, cluster headaches and migraines.
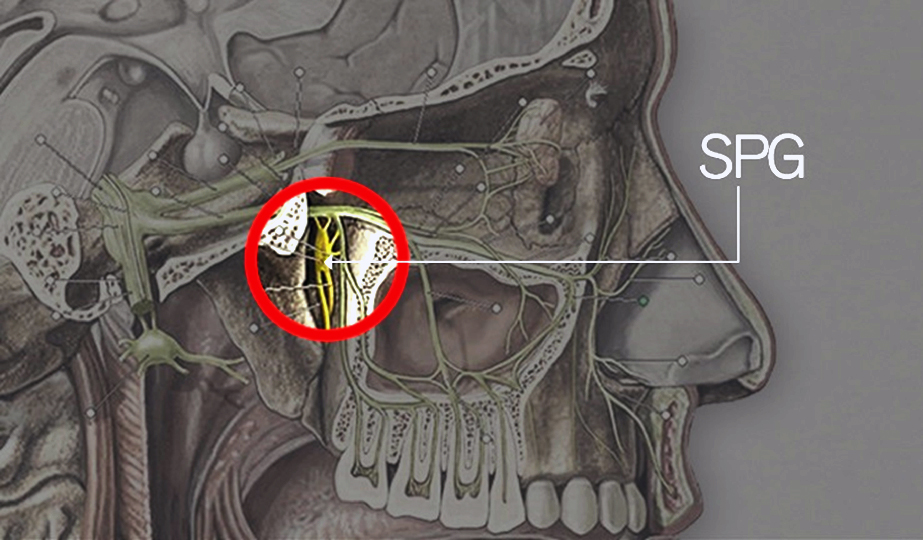
The illustration shows where the high-precision surgical instrument Multiguide injects Botox. The area is deep in the face, behind the sinuses and close to the brain. Illustration: NTNU
You may also like: Fewer headaches as you age
Long path to diagnosis
About 200 patients in Norway have the chronic disorder called persistent idiopathic facial pain. The disease is so rare and the symptoms so diffuse that it almost always takes a long time for the patient to obtain the right diagnosis. In practice, it is usually only determined after all other diagnoses are eliminated.
“A typical patient has already seen the dentist, a physiotherapist, an ear-nose-throat specialist, a neurologist, a neurosurgeon, a face and jaw surgeon, and taken epilepsy medications and antidepressants. CT or MRI images fail to detect any cause. In desperation, the patient seeks out some alternative treatment, often abroad,” says Jamtøy.
Daily life painful
As an orthopaedic surgeon, Jamtøy has welcomed patients who have had several teeth extracted to relieve pain without the pain diminishing afterwards. It’s difficult for the patient to discern where the pain is coming from, and it’s often confused with a toothache.
Severe facial pain is often incapacitating and the patient’s quality of life is significantly reduced.
Patients may have problems with daily activities. A large proportion have to quit their jobs. Unfortunately, many patients are labelled “health shoppers” and problem patients, Jamtøy says.
Often mixed up
The disorder is often confused with trigeminal neuralgia, another type of pain in the main sensory nerve of the face. This is a stabbing pain, like electric shocks that come and go. Persistent idiopathic facial pain is not quite as intense; it manifests predominantly on one side of the face, is chronic and has no demonstrable cause.
- You may also like: Do migraine sufferers have weakened blood vessels?
Operated on abroad
Some patients are treated abroad with major surgery that involves inserting an implant with a stimulator into the sphenopalatin ganglion nerve.
“The operation causes all the impulses from the nerve to the brain to be blocked when the stimulator is activated. This causes some unfortunate side effects that affect tear production and the mucous membranes of the nose and mouth. Botox has a far more targeted effect that blocks the signals we’re looking for, and it also wears off after a while.
- You may also like: Precision injections of Botox into migraine ‘centres’
Everyone who benefits treated
Jamtøy’s study is a randomized, double-blind, placebo-controlled, cross-over, pilot study. Neither patient nor therapist knows whether Botox or saline solution is being injected. The effects are recorded for five months after the first injection and before a second round, in which patients receive the opposite of what they were given in the first round. The second round is followed by three months of recording the effects.
Patients who experience a positive effect from the treatment are guaranteed further treatment.
Jamtøy is collaborating with the national treatment service for unresolved facial pain in Bergen. His advisor at NTNU / St. Olav’s Hospital is researcher Erling Tronvik.
More about the study:
Botox blokkering av dyp nerveknute hos pasienter med Persisterende idiopatiske ansiktssmerter (Botox blockage of deep ganglion nerve in patients with persistent idiopathic facial pain). In Norwegian.



