Norwegian robot hunts for the best cancer warriors
Cancer patients can regain full health with immunotherapy. Now researchers are hunting for the perfect immune cell with the help of a very special robot. No one has done this before.
Today we can program the body’s own cells to find and kill cancer cells, helping individuals who would otherwise only have weeks left to live.
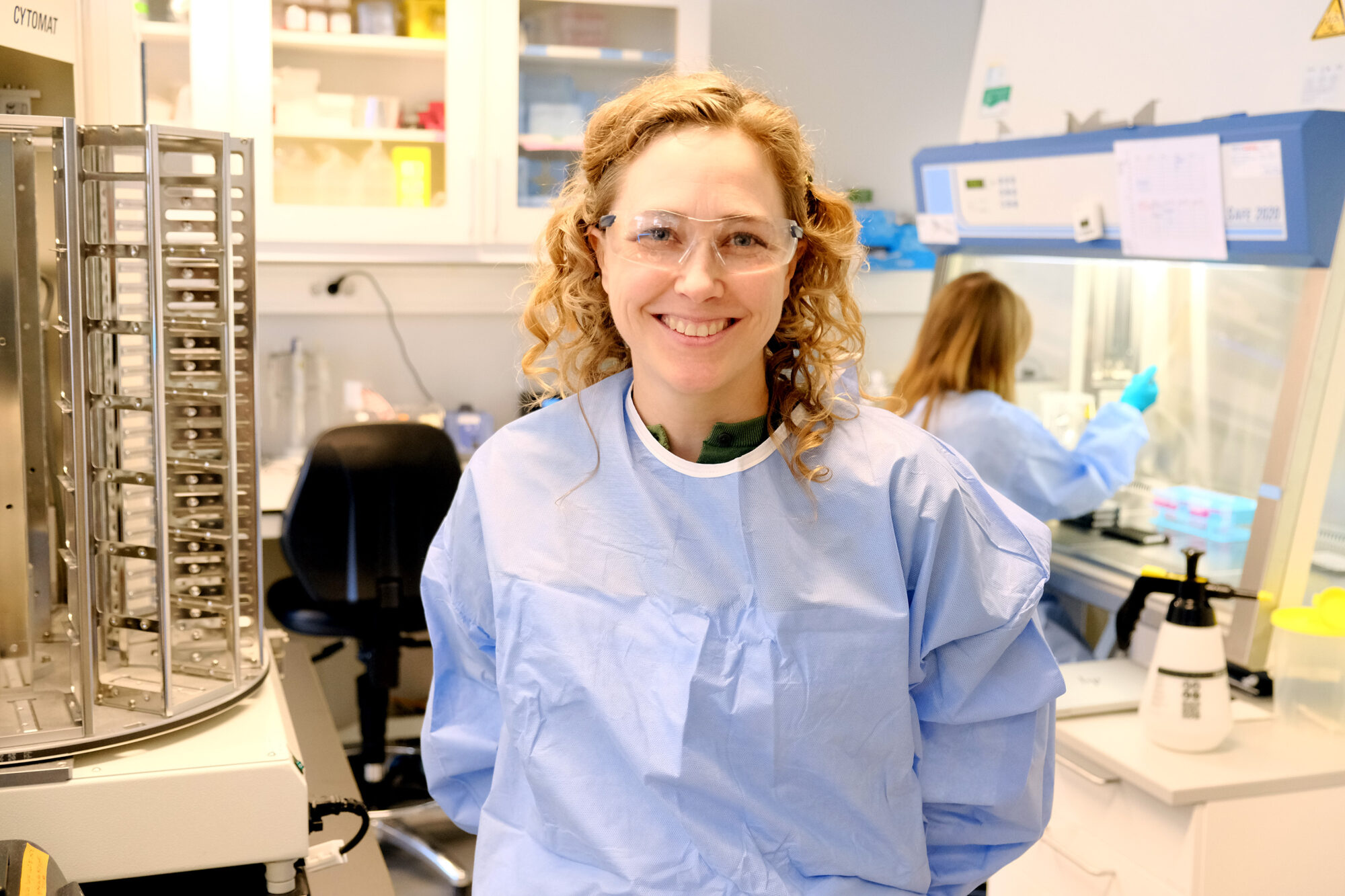
“It works. Immunotherapy is an important form of treatment that can cure cancer once and for all,” says Hanne Haslene-Hox, a senior research scientist at SINTEF.
Unfortunately, the treatment cannot save everyone. Out of 100 patients who receive this treatment for blood cancer, perhaps 40 will recover. The researchers want to increase that percentage.
The body’s elite soldiers
Haslene-Hox is talking about targeted, cell-based immunotherapy. In technical terms: CAR chimeric antigen receptor) T-cell therapy, which uses T-cells. These cells are the body’s elite soldiers and make up an important part of the body’s natural immune system.
“What we do is insert a gene that enables the T-cell to recognize cancer cells and attach to them. That’s what the body needs to recognize that ‘this is a bad guy and we’re going to take it down,’” says Haslene-Hox.
So far, these cells cannot stop a solid cancer tumour. But they work very well for blood cancer, where the cancer cells move around the body.
Only one chance
The researchers and doctors only have one chance. Patients who receive this treatment have such a short time left to live that if the therapy does not work on the first try, it’s too late to make another attempt.
“What we do is insert a gene that enables the T-cell to recognize cancer cells and attach to them. That’s what the body needs to recognize that ‘this is a bad guy and we’re going to take it down.’”
That’s why what happens to the cells from the time they are collected from the patient’s blood until they are returned to the body is so important.
Scientists still know very little about how the process itself affects the cells. They are not sure what it does to the cells’ ability to survive in the body and carry out their mission.
“The body is incredibly complex, but also very precise. When the body says, ‘we want to produce a huge amount of this cell type,’ it does it. But we’re standing there with a bowl of cells where we’ve made equal amounts of all different cell types and don’t know which one is the right one,” says Haslene-Hox.
Extensive testing work
What works varies from patient to patient. Researchers can only test a few different ways to produce the cells that will treat a patient. The laboratory contains hundreds of different additives, combinations and concentrations to choose from.
“When we collect cells from a patient, we get maybe 100 million cells. Then they are grown in their own flasks,” says Haslene-Hox.
“You want the warrior who is the best at beating the cancer, not the archivist or the retired janitor.
The job is usually a manual one: lab workers sit and distribute the cells into flasks and monitor the process.
Robots train the “elite soldiers”
The researchers at SINTEF employ robots instead. The cells that are usually grown in large flasks can instead be grown in well-like structures – plates with small depressions.

The SINTEF laboratory can test far more different ways of producing the right cells. Photo: Bjørnar Øvrebø, Innovation Norway
“Instead of distributing them across ten flasks, we can distribute the 100 million cells across 1000 wells. That gives us the opportunity to test lots of different things in a lot of different combinations,” Haslene-Hox says.
“No one has done this before. The goal is to find the T-cells that are the best warriors,” she says, once again drawing a military comparison: “You want the warrior who is the best at beating the cancer, not the archivist or the retired janitor.”
It is simply not possible to do this task manually anymore when so many different things need to be tested at the same time. The process involves taking samples, looking at each sample under a microscope, analysing them and also using up a lot of cells just for the samples. The job requires too many people and takes too long.
The only thing that works
The robot, on the other hand, is able to not only distribute the cells across a thousand wells instead of ten flasks. It can also analyse quickly, pointing out a few promising results. Then it is possible to concentrate on the variants that are most likely to work.
“No one has done this before.
“Then we can give these cells the signal that best indicates that ‘danger lurks here, so we have to make a lot of cells,’” says Haslene-Hox.
“T-cell therapy is extremely effective when it works. But the vast majority of cancer patients do not yet have immune cell therapies available to them. We have to create cell therapies that are optimally equipped to take up the fight against cancer,” she says.
Collaborating with Radium Hospital
The effective ingredients that the researchers find through the robotic screening can be relatively quickly tested on cell therapies that are currently under development – with the goal of making these T-cells as well equipped as possible to succeed in clinical use.
“This is new knowledge that can be included in the product development that researchers at Radium Hospital are already working on. These will then become part of clinical trials with new T-cell therapy,” says the SINTEF researcher.
Facts about CellFit – T-cells adapted to fight cancer:
- CellFit is a four-year immunotherapy project with the goal of finding out what is required to produce the best possible T-cells to treat cancer.
- The Norwegian Radium Hospital, which has extensive experience in developing T-cell therapies, is leading the project. SINTEF is responsible for screening, which involves examining and sorting the samples. The Oslo Cancer Cluster and Thermo Fisher are also project participants.
- The Research Council of Norway has supported CellFit with EUR 1.9 million.
References: Cellfitproject and the Research Council of Norway’s Project Bank