Psychiatric treatment no guarantee of a return to work
Mental health problems are keeping an increasing number of Norwegians out of the employment market. Treatment alone is often not enough to get people back to work. Some groups are at greater risk of being away from work for a long time – or even permanently.
Norway ranks at the very top among the OECD countries when it comes to absence due to illness and disability benefit. However, little is known about how capacity for work changes before and after treatment for mental health problems.
Researchers at NTNU have now followed more than 2600 patients with everything from mild to severe mental health challenges. All the patients received treatment in either the municipal health service or the specialist health service.
“For many people, the start of treatment does not mark a return to working life, but rather the beginning of prolonged or increasing absence,” said psychologist and PhD research fellow Jakob Lundqvist at NTNU’s Department of Psychology.
- You might also like: Many people choose unemployment benefits over poorly paid jobs
Still absent a year later
The study shows that the number of people granted sick leave increased sharply in the months before treatment began, but decreased somewhat afterwards.
Strikingly, the use of long-term benefits such as work assessment allowance (AAP) also increased. As a result, the level of absence due to illness remained relatively stable in the year following the start of treatment.
“The result was that over 30 per cent of the respondents were on sick leave, receiving AAP, or on disability benefit one year after treatment for mental health problems had begun,” explained Lundqvist.
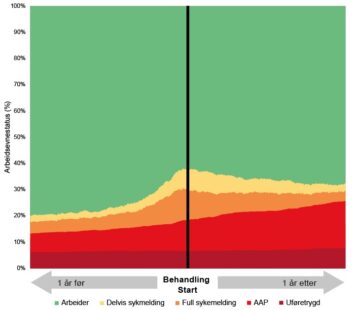
Changes in work capacity status one year before and after treatment for the entire sample of 2,609 individuals. Illustration: Jakob Lundqvist, NTNU
To understand this better, the researchers not only investigated daily status, as shown in the figure, but also the most common pathways for absence due to illness for each patient before and after treatment.
-
- IN WORK: Approximately half of the people who took part in the study maintained stable capacity for work both the year before and after the start of treatment.
- RECEIVING AAP: Approximately 30 per cent followed a pathway where their absence due to illness did decrease, but this was compensated for by work assessment allowance (AAP).
- ON PERMANENT DISABILITY BENEFIT: Approximately 7 per cent were on permanent disability benefit one year after treatment had begun. This is roughly the same proportion as one year before treatment.
Women, elderly people and specialist patients are most at risk
The analysis also found that three groups were at particularly high risk of ending up on a pathway towards increased incapacity for work:
- Women
- Elderly people
- Patients receiving specialist healthcare services
For women, the explanation may be a higher prevalence of mental health problems, gender-segregated occupations with high demands, and work–family role conflicts.
For elderly people, it is often due to slower recovery and comorbidity (the presence of two or more diseases/medical conditions in a single patient at the same time).
The fact that patients being treated by the specialist health services are absent from work for protracted periods can partly be explained by their more severe health issues. However, the situation is not that straightforward.
Waiting times can increase the risk of prolonged absence
There is much to suggest that the patient groups in the municipal and specialist health services largely overlap.
Municipalities provide low-threshold services that help patients receive assistance more quickly, whereas the referral process and waiting time before starting treatment in the specialist health service are usually longer. As a result, many people are absent from work for long periods of time before treatment begins, increasing the risk of them dropping out of working life permanently.
“This may mean that it is not just about the patients’ mental health problems, but also about how the health services are organized,” said Lundqvist.
Inadequate support
Previous research has shown that the Norwegian welfare system may also be part of the explanation for why so many people are not in work in Norway.
The schemes for sickness benefit, work assessment allowance and disability benefit provide financial security, but are not primarily designed to help people get back to work. Patients often have to manage the process themselves within a system marked by limited contact and coordination between general practitioners, the Norwegian Labour and Welfare Administration (NAV), municipal services and the specialist health services.
“This means that returning to work is left too much in the hands of the patient. For many people, this is fairly overwhelming, and it can be especially challenging for people struggling with mental health problems,” Lundqvist said.
Some GPs grant more sick leave
The GP Scheme may also play a role. In principle, GPs are self-employed with public funding, and some of their pay is determined per patient according to various rates.
A report from the Norwegian Institute of Public Health shows that self-employed GPs who earn the most from these types of rates often grant sick leave more frequently than their colleagues who receive fixed salaries. They also treat more patients and spend less time per patient.
In practice, sick leave is often the easiest option – for both the doctor and the patient.
When the system rewards short consultations and hastily granted sick leave, this can come at the expense of measures that strengthen the patient’s ability to function and capacity for work.
“In practice, sick leave is often the easiest option – for the doctor and the patient. Saying no takes more time, can lead to dissatisfied patients, and entails a financial loss for the doctor. When financial constraints, time pressure and patient satisfaction govern decisions, we risk that the long-term needs of patients receive less focus,” said Lundqvist.
- You might also like: Here’s why migraine symptoms are worse in patients who get little sleep
Greater focus on symptoms – not ability to function
Another challenge is that psychological treatment often focuses on reducing symptoms, while ability to function in everyday life and capacity for work are often not prioritized.
Lundqvist believes the healthcare system must change its perspective and make capacity for work and ability to function equally important treatment goals as symptom relief.
“Sick leave should not be seen as a form of treatment. It may be necessary, but it rarely improves the person’s capacity for work. If we are to succeed, clinicians must strengthen both ability to function in everyday life and capacity for work in parallel with symptom relief. Only then can we reverse the trend,” Lundqvist said.
References:
Lundqvist, J., Lindberg, M. S., Brattmyr, M., Havnen, A., Aasdahl, L., Solem, S., & Hjemdal, O. (2025). Work disability status following routine mental health treatment: a Norwegian registry-based cohort study. BMC Health Services Research, 25(1), 1–13. https://doi.org/10.1186/s12913-025-12856-w
Lindberg, M. S., Brattmyr, M., Lundqvist, J., Solem, S., Hjemdal, O., Roos, E., … Havnen, A. (2024). Is the Norwegian stepped care model for allocation of patients with mental health problems working as intended? A cross-sectional study. Psychotherapy Research, 35(6), 932-944. https://doi.org/10.1080/10503307.2024.2378017
Mykletun, A., Kraft, K. B., Hoff, E. H., & Østby, K. A. (2025). Fastlegenes avlønningsform og insentiver: Konsekvenser for portvokterrollen [GPs’ form of remuneration and incentives. Consequences for their gatekeeper role] (Report). Norwegian Institute of Public Health. https://www.fhi.no/publ/2025/fastlegenes-avlonningsform-og-insentiver-konsekvenser-for-portvokterrollen (ISBN 978-82-8406-492-5).
Timp, S., van Foreest, N. & Roelen, C. Gender differences in long term sickness absence. BMC Public Health 24, 178 (2024). https://doi.org/10.1186/s12889-024-17679-8
Hemmings, P., & Prinz, C. (2020). Sickness and disability systems: Comparing outcomes and policies in Norway with those in Sweden, the Netherlands and Switzerland. OECD Economics Department Working Papers, No. 1601. https://doi.org/10.1787/c768699b-en
Norwegian Labour and Welfare Administration (2024). ‘Arbeidsfokus på fastlegekontor’ – Følgeforskning av fastlegeprosjektet. Sluttrapport fra Oxford Research [‘Work focus in GP offices’ – Follow-up research of the GP project. Final report from Oxford Research]. https://oxfordresearch.no/publications/arbeidsfokus-pa-fastlegekontor