Half of all men over 60 have prostate cancer – an AI diagnostic tool could identify which need followup
Increasing use of blood tests to detect prostate cancer is leading to overworked doctors. NTNU has now created an AI diagnostic tool that can help lighten the burden.
Diagnostic tools based on artificial intelligence are now making their way into Norwegian hospitals. AI can independently read X-ray images and detect bone fractures, or assess cancer tumours in both the breast and prostate.
“AI tools can take over the detection of simple and clear-cut cases, allowing doctors to spend their time on more complex ones,” said Tone Frost Bathen. She is a professor at NTNU and the project manager of an AI-powered analysis tool for prostate cancer called PROVIZ.
Tests on patients at St Olavs Hospital indicate that the tool is very promising.
“AI can enable radiologists to determine more quickly and more accurately whether a patient needs a biopsy, and where in the prostate it should be taken from,” explained Bathen.

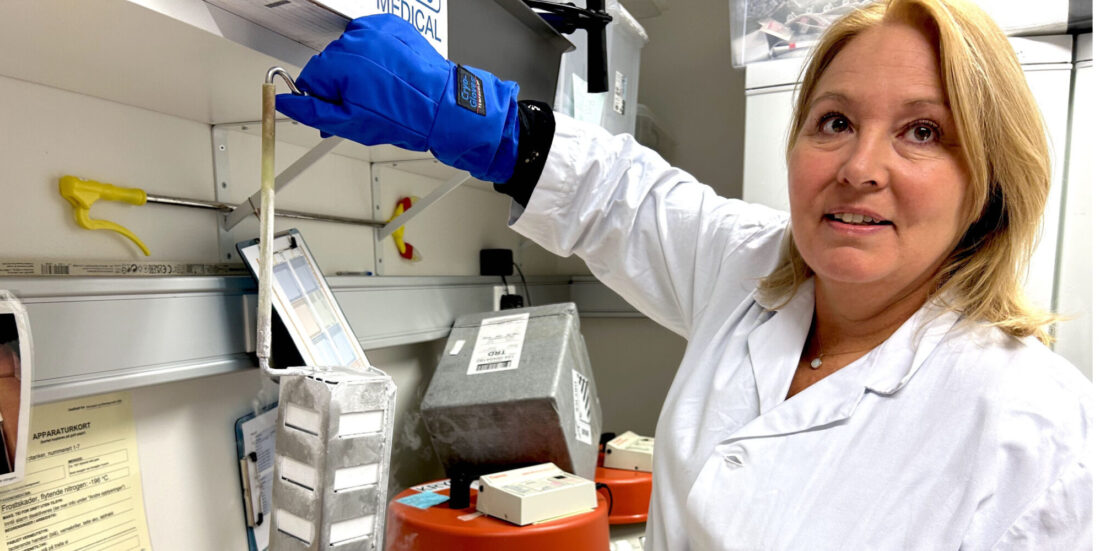
“The PROVIZ project started as early as 2018. It takes a long time to develop diagnostic tools in medicine because safety standards must be high. The application alone to be allowed to test the tool on patients was 500 pages. It is important to create a tool that clearly shows how the result was reached, and that fits into a busy hospital workday,” says Tone Frost Bathen, Professor at NTNU. Photo: Anne Sliper Midling / NTNU
A recent study shows that patients trust medical test results only if an experienced doctor confirms what has been detected.
“Trust in doctors and health professionals is key for artificial intelligence to gain a place in the diagnosis of prostate cancer. Technology alone is not enough. Human contact and professional assessment remain indispensable,” said Simon A. Berger, a PhD research fellow at NTNU.
- You might also like: Living longer with tailored chemotherapy – despite incurable cancer
Prostate cancer is a natural part of getting older
Prostate cancer is the most common form of cancer among men in Western countries.
Examinations have detected prostate cancer in 10 per cent of 50-year-olds, 50 per cent of 60-year-olds and approximately 70 per cent of men over the age of 80.
This shows that the disease is naturally linked to ageing.
“Prostate cancer is something most men die with, not from,” added Berger.
A blood test called PSA can help detect prostate cancer. Since it has become more common for men to take this blood test, the number of new prostate cancer cases has risen sharply. There are now approximately 5000 new cases each year.
When more people are tested for something that many individuals naturally have as part of the ageing process, the next medical step after the blood test must also be carried out more often, so that doctors can obtain a broader clinical picture of its severity.
- You might also like: Cancer drug can kill resistant bacteria
Most trust in doctors
Currently, this next step involves taking an MRI scan, which provides a detailed image of the prostate gland and the surrounding tissue. These images need to be interpreted manually by an experienced radiologist. As the number of images taken has increased sharply, this has created a need for new and more efficient ways of making diagnoses.
Through the PROVIZ project, NTNU researchers have developed an AI-powered tool that can help doctors interpret MRI images of the prostate. PROVIZ is currently available only for use as part of the ongoing research project, but efforts are underway to apply for a patent and make the tool commercially available.
High international competition for commercial AI tools
For a tool like this to be efficiency-enhancing in routine hospital practice, patients must also trust the findings detected through the use of AI.

“Patients have high expectations that AI can be used for faster diagnostics and to reduce healthcare waiting lists. Many see AI as a kind of safety valve—an additional resource that doctors can use alongside their professional judgment,” says Simon A. Berger, a PhD research fellow at NTNU.
Berger interviewed 18 men who had been diagnosed with prostate cancer through the use of PROVIZ. The study shows that trust in doctors and health professionals plays a decisive role in whether patients accept AI in the health services.
“Patients trust AI in lower-risk cases such as bone fractures, but not in cases where the perceived risk is higher, such as cancer. When the perceived risk is high, we place the greatest trust in specialized doctors who can confirm what AI has found,” explained Berger.
- You might also like: Peering into your heart – with the help of AI
Doctors as guarantors
In his interviews, Berger identified three different dimensions of trust.
- Foundational trust in the healthcare system: many patients had positive experiences from previous encounters with the healthcare system. This laid a positive foundation.
- Inter-personal trust in health professionals: patients trusted the doctors and their assessments. This trust was crucial for accepting AI because the doctors explained and vouched for the technology.
- Possible trust in AI: even though patients recognized the potential of AI, they always wanted a human assessment as well in prostate cancer diagnostics. They were concerned about accountability, professional judgement and AI’s (in)ability to see the whole clinical picture.
“The relationship between patient and doctor is still key. For AI to be accepted in clinical practice, health professionals must be active communicators and guarantors of safety. In order for doctors to serve as guarantors, they must first understand how AI arrived at its conclusions so they can verify that it has made the correct assessment. Patients accept the use of AI within a framework they already trust,” concluded Berger.

NTNU owns an MRI scanner at St. Olavs Hospital that is currently undergoing a major upgrade. It helps researchers obtain the best possible images to be used in, among other things, PROVIZ. “Unfortunately, there are few investors in medical technology right now, but we hope that someone sees the societal value of our project,” says Professor Tone Frost Bathen at NTNU. Photo: Anne Sliper Midling / NTNU
Source:
Berger SA, Håland E, Solbjør M. Patient Perspectives on Trust in Artificial Intelligence-Powered Tools in Prostate Cancer Diagnostics. Qualitative Health Research. 2025;0(0). doi:10.1177/10497323251387545