Plug-ins for the brain
Scientists are on the hunt for spare parts for our damaged or faltering brains. But is that a future we want?

A new beginning with a brain implant
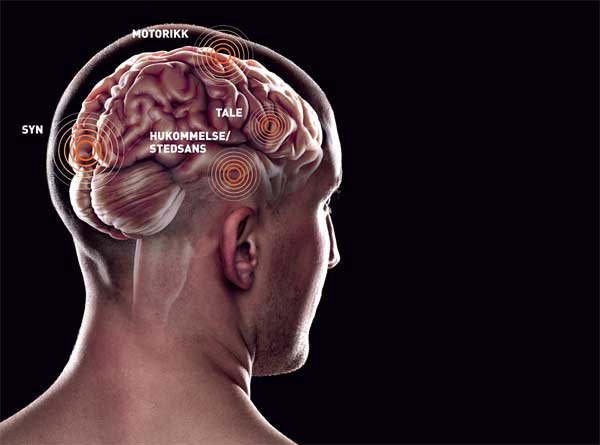
Would you give your ageing dad a new sense of location, swapped in for the nerve cells that were affected by the onset of dementia? When short-term memory fails, would it be wrong to insert a bundle of nerve cells that can give us back that skill, or that jump starts our ability to learn?
Photo: photos.com
It will not be so many more years before you will be asked to consider this question: If a loved one is suffering from a brain-related illness or injury, or is born with a brain disease – would you replace a part of her brain, if it was possible? And would she still be the same afterwards?
I spent most of the summer of 2011 in a sweaty chair, next to a hospital bed. There lay a beloved family member who was left to the best that St. Olavs Hospital in Trondheim had to offer. An operation did not go as planned, and his life and mind hung by a thread – or more accurately, by plastic tubes filled with blood, medicines and oxygen.
As our patient’s consciousness slowly returned, our family’s uncertainty grew: Would he recover? And would he be the same person?
When your loved ones suffer from disease or injury, you are often willing to try any treatment. No question about using medications that affect the brain – but what about a transplant?
Would you give your ageing dad a new sense of location, swapped in exchange for the nerve cells that were affected by the onset of dementia? What about memory? When short-term memory fails, would it be wrong to insert a bundle of nerve cells that can give us back that skill, or that jump starts our ability to learn?
Is this just a pipe dream, or is the ability to supply replacement parts to the brain closer than we think? Is brain transplantation just around the corner?
In the end, it all went well with my family member. But my questions did not disappear. I decide to hunt down the truth about replacement parts for the brain.
The gas pedal and brake
I have heard that the brain has an extra level of protection, so my first step is to talk to a woman who can say something about the brain and the body’s immune system. Carla Shatz, a professor of neurobiology at Stanford University in the United States, discovered that nerve cells produce the molecules that the body’s immune system uses to recognize enemies.
Enter the bioprinter
 Brain researcher Ioanna Sandvig at NTNU can imagine a future where we can print out replacement pieces for the damaged areas in the brain.
Brain researcher Ioanna Sandvig at NTNU can imagine a future where we can print out replacement pieces for the damaged areas in the brain.
VIDEO: Organ printing(youtube.com)
Shatz and her colleagues have set a goal to find out how our experiences influence the development of the nervous system. Through studies of the visual system, they found that the very genes that are used in the body’s immune system are also the switches that regulate the development and adaptation of the brain’s networks.
“Initially, we believed that the brain was ‘immune privileged’, which means that it does not express the same kind of immune response as the body,” says Shatz. “In that way, it would actually be easier to transplant tissue into the brain than in the rest of the body. But then we discovered that the brain still produces what are called the MHC class 1 molecules. The difference is that the brain is not the same as the body.”
“This gene, MHC, works in such a way that if you turn it off, it’s like removing a brake on learning,” she explains. “And in the animal experiments we have done so far, what we call plasticity, the brain’s capacity to create new connections, is much greater when we remove the MHC brake. This is also true in older animals.”
New cells, new life
Shatz explains that once they have a complete overview of the accelerators and brakes in the brain, it might be possible to jump-start the capacity of people to learn, even for elderly.
“What if we could give a stroke patient a pill that gave the brain a chance to learn again?
Something that would let the areas not affected by the stroke to connect and take over the functions of the stroke-affected area?” she says. “Or think of the children with cerebral palsy whose ability to learn is impaired. What if their learning ability could be improved, which would give them a better life? Wouldn’t that be wonderful?” she asks.
I can’t disagree. All this is possible in the future, Shatz thinks. It may be appropriate to treat patients with a mixture of specialized stem cells in combination with medication. This could improve the brain’s ability to link new neural systems with existing ones.
As early as 1998, doctors attempted to help a patient with Parkinson’s disease by inserting new cells in the brain. It was hoped that these new cells would replace old ones that no longer produced the neurotransmitter dopamine. This was the first step in nerve cell transplantation, and produced good results, but also had some side effects. So perhaps it’s not as simple as just inserting fresh, hard working cells into the brain.
The dream of a bioprinter
New nerve cells on the way
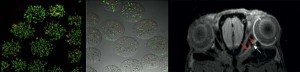
If the optic nerve is damaged, you can’t just send in replacement cells. Alginate researchers and scientists from the MI Lab at NTNU are collaborating on the development of small spheres that can serve as artificial wombs for nerve cells. These spheres provide nutritious substances in a soft, supportive environment where new nerve cells can grow. Different magnetic resonance imaging (MR) techniques enable the researchers to monitor the growth process carefully. To the right is an MR image of an injured rat optic nerve (red arrows) with new nerve cells that are being followed closely by researchers (white arrow).
In my search for answers, I happen to meet Greek-born brain researcher Ioanna Sandvig. She transformed herself from an economist into a biologist at Imperial College in London, after having discovered her love of neurobiology and a Norwegian researcher.
Sandvig has just submitted her PhD thesis in neuroscience at NTNU. I meet her at the MRI centre at St. Olavs Hospital. She presents a perspective on replacement parts for the brain that I have not been imaginative enough to think about.
“Sometime in the future – I don’t know when, but it’s what we are working towards – I can imagine that a patient comes in with an acute brain injury, and is sent for a scan,” she says. “At the same time we take skin tests or at least some cell samples. This gives us the genetic information that makes it possible to design cells from scratch, to match the patient perfectly. Then we get a three-dimensional picture of the damage from the scan. We then send this information to a bioprinter that can print a substitute piece for the damaged area.”
Well, I think, that’s something. It’s one thing to realize that there are actually “printers” in the United States that can actually “print out” fresh skin for soldiers injured during war. This is possible to imagine. But how likely is it, really, that we will be able to print out customized brain parts?
Sandvig calms me down with the reminder that it will be decades before we see a glimmer of this kind of custom repair. And on our way, we have a lot to learn and many puzzles to solve.
Alginate womb for brain cells
Ioanna Sandvig and her colleagues are focused on how to make the optic nerve grow back together if it is damaged. It’s harder than you might think, to make repairs inside the brain. The nerves not only have to overlap, but they are also dependent on a sophisticated support system. The researcher compares this kind of repair work to getting a car to cross a road that has been destroyed by a flood.
“If the road is destroyed, it does no good to refuel the car,” she explains. “You have to redo the gravel foundation before you can top the road with asphalt, and only then can the car cross the road. It’s the same with nerves that are cut. Both the nerve and everything around it have to be cared for in the right order. It is incredibly complicated. It is not enough to simply have the right replacement cells.”
At NTNU’s MI Lab (Medical Imaging Laboratory), where Sandvig works, researchers have established a broad scientific network that involves many other disciplines. In collaboration with alginate researchers, the MI Lab is helping to develop small spheres that enclose a soft, supportive environment with lots of nurturing substances for nerve cells or other cell types to grow.
“These tiny balls are like little wombs for the cells,” says Sandvig. “The cells are provided an optimal environment. This increases their chance of survival when they are inserted into the brain.”

VIDEO: DARPA prosthetic arm (youtube.com)
A bioprosthetic arm
Through a DARPA research project called “Human Assisted Neural Devices” (HAND), researchers have developed a prosthetic arm that is almost like a new biological arm. This arm is controlled directly from the brain via the recording of brain waves from sensors that are placed directly on the brain surface. In time, the project’s researchers hope to create memory prostheses that could give memory back to soldiers injured in combat.
Photo: UPMC
The MI Lab follows the newly grown cells closely using different MR imaging techniques.
“One type of image follows the development of the cells we insert. Another type can be used if the torn nerve fibres begin to send out new shoots and grow. This way we can track and monitor the growth process,” explains Sandvig carefully.
I wonder aloud if she will be able to make moulded clumps of cells soon. And if she believes that we will some day be able to make spare parts for the brain. She answers with certainty:
“It will probably be many decades before we get there. But we will get there!”
Nanoparticles
In a few decades, yes. That’s about when the elderly wave will crash over us with full force. In 2050 there will be close to 160 000 people with dementia in Norway, if the statisticians are right. That is well over twice as many as today. And they will all require their share of nurses, nursing homes places and health care expenses, respectively.
Most people who develop dementia have Alzheimer’s disease. It is usually detected when a person’s sense of place and short-term memory deteriorates drastically. A group of researchers in Trondheim have worked for some time to understand these two aspects of the brain in detail.
May-Britt and Edvard Moser are co-director and director of the Kavli Institute for Systems Neuroscience at NTNU. Their research has shown how nerve cells in a specific area of the brain store memories, make similar memories different, enable us to pick memories up again, and how this all connects with our sense of place – and about which they have also uncovered fundamental principles.
But what do they think about the possibility of replacing damaged parts of the brain with new parts?
“Transplantation has been underway for some time, in the form of what are called grafts,” Edvard Moser responds.
“Look at the use of stem cells in the brains of patients with Parkinson’s disease. We’re already ‘transplanting’ cells to compensate for declining function.”
Moser points out that there are also more and more examples of electronic prostheses that work with the nervous system, such as cochlear implants for the ear and mechanical hands. Maybe the brain can eventually be filled with functional electronics?
“We can probably get the brain to interact with electronic circuits,” Moser says. “But I do not know of any interfaces yet. Generally, the more specific tasks and the fewer cells and functions involved, the more realistic the idea.”
Moser does not think we can transplant large sections of a brain.
“That’s a lot to ask, because everything would have to be connected with the rest of the brain in the right way, at least based on what we know today. But I think probably that we may someday transplant cells or nanoparticles that perform specific tasks in the brain,” he says.
Gadgets that build bridges

An electronic voice
Steven Hawking suffers from a rare variant of amyotrophic lateral sclerosis (ALS). The disorder ties him to his wheelchair, and makes it impossible for him to communicate directly with the outside world. He works with a specially designed electronic voice synthesizer and computer program that is controlled by his eyes and certain muscles in his face.
Photo: wikipedia
But there are those who believe that transplantation could be a reality, including scientists at a US military centre for advanced research known as DARPA (the Defense Advanced Research Projects Agency).
Through a DARPA research project called “Human Assisted Neural Devices” (HAND), researchers have developed a prosthetic arm that is almost like a new biological arm. This arm is controlled directly from the brain via the recording of brain waves from sensors that are placed directly on the brain surface.
The HAND project is now moving forward with the detailed mapping of how short-term memory works. The goal is to help repair the memories of soldiers who are injured in combat, by creating “gadgets” that can bridge damaged parts of the brain.
We can also hope that any technology that will provide soldiers with memory implants will also someday be available to civilians who struggle with losing their memory.
An ethical problem?
So far there are more challenges than solutions. But no one disagrees with the overall trend: Someday there will be replacement parts for the brain, in all shapes and sizes.
But what do we do when the day comes and our sense of place no longer works – but we have a brand new replacement part ready to plug in? Do we just plug it in? Or does this pose an ethical problem?
Leif Edward Ottesen Kennair is an associate professor of psychology at NTNU. He is an evolutionary psychologist, and is interested in human nature. I ask if he would recommend that we use replacement parts for the brain.
He responds with a clear yes: “We already do this for hearing. And who would consider the use of crutches a moral dilemma? If they are genuine replacement parts, then they merely replace a lost function. I think from a medical ethics perspective, you have to say yes to their use.”
The use of replacement parts does not raise major ethical questions for the psychologist.
“I imagine that one could create mechanisms to replace lost processes,” he said. “If it is possible to actually grow new nerves, it may not be necessary to map out the brain in such a detailed mechanical manner. It might be enough to get cells to grow that have a specific function. For me this is not about ‘tampering’ with brains or people, it’s about replacing lost abilities with similar capabilities.”
Nevertheless, Kennair is not convinced that we will have replacement parts very soon.
“There is so much that has to be clarified before we can come to any conclusions,” he said. “It’s one thing to create an anatomical model of the physical brain, and of how nerve cells are connected together and communicate. But the question is whether researchers can also manage to create an artificial brain that also works functionally. Otherwise, you’re left with a very advanced spaceship that you have no idea how to fly.”
“We should certainly be able to describe the brain. But we psychologists are working to answer the question ‘What is the brain actually doing?’”
What about the soul?
Imagine that our loved one’s brain is gradually refreshed with new nerve tissue. What about the day when my mom seems in fine shape after a brain operation, but has forgotten who her children are? Does she have dementia or she is healthy but with a new consciousness?
“New nerve tissue is not replacement tissue, it is a healed body part,” says Kennair. “It is organic, not mechanical. I think in the case you describe, that your mother will experience things again and will learn, and she will be considered to be much the same as someone who has ‘natural’ memory loss. The degree may be mild to severe, but now she has the opportunity to learn and remember again.”
But what about the soul, I ask.
Hjernen neste steg
 Robin Martin Kåss, State Secretary for the Norwegian Ministry of Health and Care Services, says that we have made very significant progress in treating cancer and cardiovascular disease, but have not made the same progress in brain diseases.
Robin Martin Kåss, State Secretary for the Norwegian Ministry of Health and Care Services, says that we have made very significant progress in treating cancer and cardiovascular disease, but have not made the same progress in brain diseases.
Photo: Magnus Ridola, MOH
Resources and justice
Philosopher Allen Alvarez at NTNU studies the ethical aspects of improving human beings. He thinks that solely looking at one person’s case, and his or her possible improvement through a brain transplant is too narrow a view. Instead, he says, we need to consider both resources and identity.
“It requires huge sums of money to discover and develop what it takes to succeed in growing nerve tissue or to perform transplants,” Alvarez says. “It then becomes a question of allocation and justice, particularly if this is money that would otherwise be spent on treatments that have a known and proven effect.”
“Is there a principled way to decide whether we should invest large sums in developing future medical technology, for example, rather than spend the money for expanded health care services in our own or other poor countries?” the philosopher muses.
Alvarez believes that there are several factors that influence whether it is morally right to invest in the development of technologies such as brain transplants. “The size of the need, and what it will cost us as a society, come into play,” he observed.
The philosopher then presented a completely different problem that had nothing to do with resource allocation, but about you as a person, and your identity: who you are.
Only biology?
“When it comes to consciousness, we do know not enough to determine whether there is something that can be moved with a brain or not,” he says. “This is a controversial matter no matter which field you view it from, and is far from being understood. Is the brain the basis of consciousness alone, or is consciousness the result of the interaction between the brain and body?”
Alvarez proposes a thought experiment. “What if we could transplant awareness alone,” he suggests. “Maybe upload it to a computer? What is it that makes you yourself, your identity? Is it the brain alone? The brain and the body? Do the mind and body have to live in and relate to the environment to exist?”
These kinds of thought experiments can give you a headache just to think of them. And Alvarez has several other ethical issues to ponder:
“What about decisions?” he asks. “Who should decide whether a person should undergo brain surgery that involves a transplant if this person is not able to make decisions on his or her own? What will we say on the day someone wants to do a performance-enhancing transplant? How about having to undergo transplantation, if this proves to be the best or most inexpensive treatment method – should we be able to refuse?”
As we learn more about the brain, the philosopher says, our ethical dilemmas change in step with changes in the perception of ourselves as conscious human beings.
Not immoral
 Leif Edward Ottesen Kennair, an evolutionary psychologist at NTNU, thinks it’s perfectly fine to use replacement parts in the brain: “We already do it with hearing. And who would turn the use of crutches into a moral issue?
Leif Edward Ottesen Kennair, an evolutionary psychologist at NTNU, thinks it’s perfectly fine to use replacement parts in the brain: “We already do it with hearing. And who would turn the use of crutches into a moral issue?
Photo: Mentz Indergaard/NTNU Info
Alvarez is now working on a project where he and colleagues from the University of British Columbia are examining what people think about performance-enhancing, or body-improving measures. Next year we will know how the younger generation addresses the dilemmas surrounding life-prolonging medication; whether they will accept radical synthetic treatments, nano-technological implants, or just natural implants; what they think about population growth if we all were to become significantly older; and a number of other issues that we are likely to face in the coming decades.
A luxury problem
I am increasingly at a loss. How can we make the best decisions? And what should we prioritize?
Health also concerns politics, so I contact Robin Kåss, State Secretary for the Ministry of Health and Care Services. With a background as a general practitioner, he has faced his share of elderly individuals who feel that their brains are beginning to fail.
“We are aware that mental illness is a growing problem, not least due to an ageing population,” he said. “Therefore, we already have a sharper focus on this issue in our Neuroplan 2015, and are actively participating in the establishment of a joint programme for dementia research in the EU.”
“The main problem today is that there is no significant degree of curative treatment, i.e. treatment that makes you healthy and doesn’t just relieve some of the symptoms,” he said. “We have made very significant progress in the fight against cardiovascular disease and cancer. But we have not had the same progress when it comes to brain diseases.”
Kåss thinks one of the greatest challenges is that because we live longer, there will be more and more people with dementia. I ask what he thinks will happen on the day the opportunity presents itself to replace the diseased brain cells of an Alzheimer’s patient with healthy brain tissue pieces. Will this be the solution that gives older people more good years, and shortens the lines for nursing home places?
“When so many people suffer, the most important challenge is to find new knowledge, to gain a greater understanding of the brain,” says Kåss. “There is no doubt that new therapies will challenge us and raise ethical questions. There may be a need for a thorough debate, and the Norwegian Storting (Parliament) will have the final say in the matter. We’ll take it as a luxury problem the day that this kind of treatment is available.”
The pharmaceutical industry

Savings abound
Brain disorders cost Norway NOK 78 billion each year, according to a new European report on the costs of brain diseases in Europe. This also includes the indirect costs that are estimated to total 40 per cent of the 78 billion, such as work absences, impaired functioning and similar conditions.
Photo: Geir Mogen
So the question is whether money will be the reason that prevents the development of new treatments for brain diseases. A new European report on the cost of brain diseases points to two worrying trends: The pharmaceutical industry moved out of Europe to the United States, China and India because Europe cannot agree on patent and approval systems for pharmaceuticals. At the same time, industry is disappointed with the return on investment in research on brain diseases, the report said. It has also proved difficult to conduct good research on these diseases, and it is generally difficult to obtain approval for treatments that affect the central nervous system. This means that several pharmaceutical companies have completely stopped their involvement in brain research.
Karita Bekkemellem, administrative director of the Association of the Pharmaceutical Industry in Norway (LMI), believes that it is by no means the pharmaceutical industry that stops the development of new drugs to replace established treatments.
“The pharmaceutical industry works continuously with new drugs for diseases for which there is already a treatment, not least because both the government and patients require more and better and safer drugs. Thus there will always be competition for established treatments,” she said.
“Normal market mechanisms work, where a pharmaceutical company develops a drug that will compete with products from another company. At the same time the companies will develop and make their own medicines better and more cost effective so that they continue to be the preferred treatment,” says Bekkemellem.
She tosses the ball to the authorities.
“Based on the goal that research should constitute three per cent of GDP, the government cannot be particularly happy either. A greater focus on future-oriented biotechnology can provide a significant increase in research in Norwegian industry, while it allows for more medical advances,” Bekkemellem says.
Frankenstein’s monster?
I have talked with many wise people. But I still do not know if we – if and when the time comes – will seize the opportunity and not look back. Or if we really should think things through first.
Because it’s a little scary, undeniably so, to tamper too much with the finest organ we have. What if we lose control? What if we inadvertently create a monster, like the Frankenstein scientist Victor does in Mary Shelley’s novel from 1818, where he creates a new being made of body parts from dead people?
It may seem as if the fear of losing control of a person’s personality, and ending up with something that is worse than we had at the start, is at the core of the opposition to tampering with the brain.
This has not stopped scientists, however. Just fifty years ago, the United States and the then Soviet Union were engaged in a fierce battle as to who would be the world leader in the sciences. In a variety of sometimes grotesque film clips that are openly available on the Internet, we can see how both American and Russian scientists documented their experiments with head transplants, or full body transplants as they were fondly called.

Dog heads and hype
In Russia in the 1950s, Vladimir Petrovich Demikhov conducted experiments on dogs. He detached a dog’s head from its body and kept it alive, just connected to a blood pump. Later, he transplanted a puppy’s head onto the neck of an adult dog. In one of the films from his laboratory, we can see the transplanted puppy head and the adult dog drinking simultaneously from their own bowls.
Photo: Wikipedia
In the Soviet Union in the 1950s, Vladimir Petrovich Demikhov conducted experiments on dogs. He detached a dog’s head from its body and kept it alive, just connected to a blood pump. Later, he transplanted a puppy’s head to the neck of an adult dog. In one of the films from his laboratory it’s possible to see the transplanted head on the puppy and the adult dog drink from their separate bowls, simultaneously.
Human hearts, ape heads
The South African surgeon Christiaan Barnard considers Demikhov to be a teacher and an inspiration. He also visited Demikhov’s laboratories twice. In 1967 Barnard gave a 54-year-old vegetable trader named Louis Washkansky an early Christmas present in the form of a new heart. Washkansky died 18 days later of pneumonia, but this was the first successful heart transplant in a man. Today global heart transplantation has reached a scale that there are about ten heart transplants undertaken every day. The person who survived the longest with new a heart had it for more than thirty years.
Dr. Robert Joseph White, an American organ transplant pioneer, also visited Demikhov’s laboratories. White is probably the first American who studied Lenin’s brain.
Inspired by Demikhov’s work, White moved the head and brain of a monkey to another monkey’s body. It was a full day’s work for a number of surgeons to connect the corculation systems between the head and the new body. In an interview, the late Dr. White described how he felt minutes after the operation:
“We saw electrical activity that was being measured in the brain. It was like walking through a barn dance, everyone was ecstatic. Eventually we could see that the anaesthesia was wearing off. We saw that the eyelids began to move and the lips began to move. The animal was awakened. It was not a happy animal, I could see. We took the eraser side of a pencil and touched the teeth of the monkey, and it bit the pencil. We rang a bell, a sound that monkeys don’t like. We saw a reaction. That night I realized that we had completed a monumental achievement, whether good or bad. I realized that what we had done for the monkey, we could also do for humans,” said Dr. White.
This was in 1970. The monkey lived on a few days and was, as far as Dr. White knows, conscious to the same extent as before the surgery. But the monkey was paralyzed from the neck down, because its spinal cord was cut.
VIDEO: Headtransplant on an ape. Warning – strong visuals. (youtube.com)
White was the medical consultant on the film “The X-Files: I Want to Believe,” and founded Pope John Paul II’s Committee on Bioethics. He was a kind of neurosurgery elderly statesman and had as his motto to promote the right to life for all ages.
Neural prostheses
In the 1970s and beyond, there were experiments with many types of neural prostheses. In 1978, William Dobelle developed the first artificial eye.
Admittedly, the “eye” was only 68 electrodes that were connected directly to the visual cortex of a man, “Jerry,” who had become blind as an adult. And “Jerry” did not get his vision back, but he did have the experience of seeing flecks of light.
In 1998, scientists succeeded in linking the brain with electrodes in such a way that a patient was eventually able to control his computer mouse cursor with his brain alone. The patient, Johnny Ray, was “locked” in his own body without the ability to move, after he had a stroke in his brain stem. That same year, specialized nerve cells that produce the neurotransmitter dopamine were for the first time ever inserted into the brain of a Parkinson’s patient to replace damaged cells.
Over the last ten years, more and more advanced prostheses have been produced.

Tailor-made brain implants
It’s possible now to print out a kind of skin – layer by layer – that can be placed directly on a wound. In the future it is hoped that doctors will be able to print out whatever body part or brain part you need.
Photo: Gismag
Prostheses with good connections between nerve cells and electronics have given humans functional artificial hands.
The latest version of this kind of hand is controlled by thought alone.
And for the first time this autumn, a trial was approved that will involve the insertion of stem cells to heal damaged spinal nerves in humans. The treatment has been promising in animals, but it will nevertheless be some time before people can walk away from their wheelchairs as a result of stem cell therapy.
Man and machine
A good example of human-computer interaction is the famous British mathematician and astrophysicist Steven Hawking. Hawking suffers from a variant of amyotrophic lateral sclerosis (ALS), which ties him to his wheelchair and makes it impossible for him to communicate directly with the outside world. Hawking uses a custom-made electronic voice synthesizer and computer program that is controlled by the eyes and certain muscles in his face. The electronics thus allow him to “speak”.
Interaction between the brain and electronics is also common in the world of computer gaming. In a game called Mind Flex, a player wears a special headband that enables his or her brain waves to control the movement of a ball through an obstacle course.
A synthetic brain
The first major project designed to create a complete synthetic brain is the European Blue Brain project, which began in 2005. Three years later, scientists had finished constructing the first bit of brain, with 10 000 cells. In July 2011 they had increased this to a neural circuit with a million cells.
Blue Brain has now moved into a new phase. In a continuation of the Human Brain Project, a large European collaborative project with 13 research partners from nine European countries, the goal is to have built a complete model of the human brain in 2023, with one hundred billion nerve cells.
And here ends my quest for the artificial brain. Whatever we may think about the issue, all indications are that we long ago entered an age where the brain is no longer the last impregnable jungle. Quite to the contrary, it is being mapped and understood.
And with that, help for your brain will be coming to your neighbourhood sooner than you might think.