Answer to the blood pressure mystery could lie in our genes
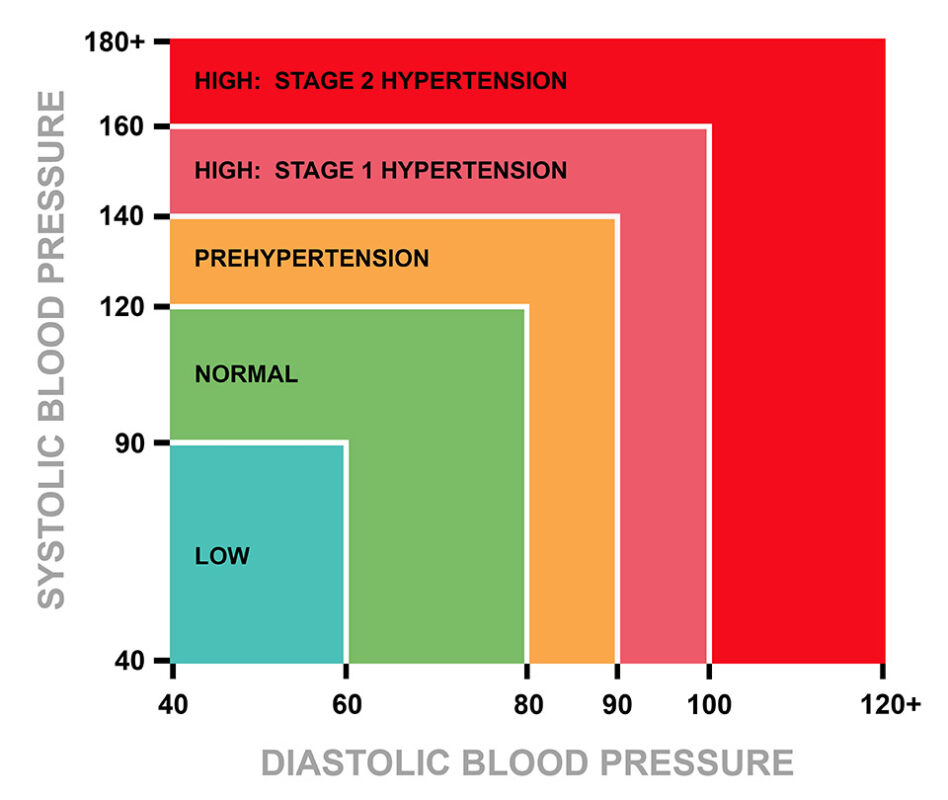
Hypertension affects one billion people and is considered the number one cause of death worldwide. Mass testing of genetic variants can now shed light on the cause of high blood pressure.
High blood pressure is often called the silent killer. Globally, more people die each year from cardiovascular disease than from any other disease.
High blood pressure – or hypertension – increases the risk of heart disease, kidney failure and stroke. Yet, the health system estimates that only half of all the people with hypertension are aware of having it themselves.
Only half of those who are aware of it and receive treatment have their blood pressure under control.
“Blood pressure research is a huge field,” says Rune Mo, a cardiologist and associate professor at NTNU.
Thousands of scientific articles on hypertension are published every year. It is well known that hypertension “runs” in families. However, researchers have not been able to point to one specific cause of the disorder.
Only in ten to fifteen per cent of cases are the underlying causes known.
“Blood pressure is the mechanical pressure that the blood exerts on the blood vessels, and which is necessary for the blood to flow through the vascular system. Blood vessels are elastic. They can expand and contract so that the pressure isn’t too high or too low,” says Mo.
Despite complex and advanced regulatory mechanisms, some people’s blood pressure stays so continuously high that blood vessels and organs are damaged.
- You might also like: Lifelong marriage lowers risk of dementia
Like a thermostat turned up too high
The reason that the direct cause of high blood pressure has not yet been determined might well be because so many different mechanisms in our body influence it.
Our autonomic nervous system is the key to regulating blood pressure and other unconscious tasks that are not directed by our will.
The autonomic nervous system enables the body to cope with various challenges, like keeping the body’s basic functions in balance and regulating our body temperature, breathing, digestion – and blood pressure.
Imagine a person who is surprised by a storm in the mountains and sitting in the snow and freezing. The person’s sensory cells register that the body’s core temperature is dropping.
The cells send a nerve impulse to one of the centres in the brain, the hypothalamus. Here, the body’s temperature is then compared with the biological thermostat, which is set to 37 degrees Celsius.
The hypothalamus then acts to raise the body temperature. It might send nerve impulses to the vascular system under the skin with a message to contract and for the muscles to start trembling.
Regulating blood pressure follows the same pattern. We have nerve cells in our heart and blood vessels that monitor blood pressure by registering the stretch in the heart and artery walls. These nerve signals are sent up to a separate centre in the brain.
If the signals report that the blood pressure is lower than the pre-set value, the centre will tell the blood vessels to constrict and the heart to increase its frequency and stroke volume, causing blood pressure to rise.
“If you have a family history of high blood pressure, it’s as if this thermostat is turned way up,” says Mo.
- You might also like: Diabetes detection is far better than has been feared
Salt is the crux of high blood pressure
Nerve signals from the blood vessels are only one of the triggers that cause the veins to contract.
“If blood pressure drops or the kidneys have a reduced blood supply, the kidneys will secrete the enzyme renin. Renin causes the arteries to constrict via a hormonal cascade, which increases the resistance in the blood vessels so the blood pressure rises.
Too much salt in the blood can cause the blood pressure to become too high, and reducing the salt content in food has long been recommended to address high blood pressure.
Our blood pressure is also affected by blood volume.
“A person who becomes dehydrated or loses blood causes the volume of blood to decrease and the blood pressure drops. In severe cases, health personnel will administer saline fluid or blood intravenously to prevent the blood pressure from becoming too low. Intravenous drugs that constrict the blood vessels can also be used,” says Mo.
Too much salt in the blood can cause the blood pressure to become too high, and reducing the salt content in food has long been recommended to address high blood pressure.
Salt binds water and increases blood volume. Salt can also contribute to constricting the blood vessels and thus increase blood pressure.
Chinese writings dating back to 3500 BCE even make mention of salt affecting blood pressure. “Too much salt makes the pulse hard,” they wrote.
“Many people with high blood pressure are salt sensitive, but not all. Some are vulnerable to effects of high salt intake, others less so,” says Mo.

Despite complex and advanced regulatory mechanisms, some people’s blood pressure stays high continuously so that blood vessels and organs are damaged. Photo: NTB, Shutterstock.
Salt stored in the skin
Just why salt increases blood pressure is still not known. About half of all people are salt-sensitive, meaning that they experience changes in blood pressure when their salt intake varies.
This suggests that part of the solution to the blood pressure puzzle lies in how the body handles salt, says Helge Wiig, a professor at the University of Bergen.
“Large population studies have shown a connection between salt intake and blood pressure. If you have a hereditary condition where you respond to changes in salt intake, it can increase your blood pressure by as much as 10 per cent. But we’re talking about a complex connection,” says Wiig.
Sex hormones could be involved as well. In women, you often see an increase in blood pressure after menopause.
Wiig and his colleagues in Bergen have chosen to study the skin’s role in regulating blood pressure. More recent research shows that this organ might play a hitherto unknown role.
“The kidneys are the major organs involved in regulating the body’s salt balance, but we and other researchers have findings indicating that salt can be stored in the skin. It seems the skin acts as a kind of buffer,” says Wiig.
Skin a barrier to fluid loss
Salt consists of the two substances sodium and chloride. Animal experiments now show that the sodium ions are taken up by cells in the skin, in exchange for potassium ions. The so-called osmotic pressure in the cells thus does not change, and the local fluid balance is maintained. The blood pressure rises in response.
Skin serves as a barrier to fluid loss and might thereby influence blood pressure.
“What we’ve found is that we have an intracellular storage of salt, another way of saying that sodium is stored in the cells. This happens not only in the skin but also in the muscles,” says Wiig.
The researchers also believe that the skin serves as a barrier to fluid loss and might thereby influence blood pressure.
“As you age, the skin no longer performs this barrier function as well, and you can lose more water through the skin than when you were younger. This is one of the reasons why older people can easily become dehydrated. The body protects itself from losing water through the skin by constricting the blood vessels. When the blood vessels constrict, the blood pressure increases,” explains Wiig.
Answer to high blood pressure may lie in the genes
Along with high salt intake, a number of other risk factors are known to affect blood pressure. Obesity, smoking, excessive alcohol intake and lack of physical activity are high on the list.
So how do we know whether a person’s risk of high blood pressure and cardiovascular disease are the result of years of excessive salt intake, smoking or being a couch potato, or whether we are simply born that way?
“We talk about having a genetic susceptibility. But genetics in relation to blood pressure is complex, because so many different systems and interactions between the systems play in. Researching genetics and hypertension is almost like going for a walk in the woods. You see something here and something there, but you don’t quite know what it all means,” says Mo.
An increasing number of researchers nevertheless believe that the answer to the blood pressure riddle lies precisely in the genes – at least partially. We react differently to salt, for example, depending on what genes we are equipped with.
“High blood pressure is at least partly genetically determined,” says Knut Erik Berge, a specialist in medical genetics at Oslo University Hospital.
Studies have shown that hereditary factors contribute to between 30 and 40 per cent of blood pressure variation in the population. However, only in a small number of cases can one point to a specific gene and say exactly where the problem lies.
“We have a genetic group in the population that has what can be called a monogenic form of hypertension, but that’s very rare. In the vast majority of cases, the increase in risk is a matter of having a combination of genes in conjunction with lifestyle factors,” says Berge.
- You might also like: Yes, it’s true: A walk in the woods actually helps with anxiety and depression
More than 1500 genetic variants
Nevertheless, knowledge of the monogenic forms – cases where only a single set of genes is involved – can help to shed light on the blood pressure mystery.
“If you have a mutation in a particular gene, and this causes high blood pressure, then understanding the genetic mechanism can also provide knowledge about what causes hypertension in general,” says Berge.
Having a combination of several of these ‘unfortunate’ variants could explain why some people have higher blood pressure than others.
An example is Liddle syndrome, which is caused by a mutation in a single gene that codes for a protein in the kidneys. The protein is part of a mechanism that causes the kidneys to increase the amount of salt in the blood, and carriers of this gene often suffer from severe high blood pressure already at a young age.
Today, inhibition of this protein is a known mechanism for treating hypertension, even if the patient does not have Liddle syndrome.
“About 30 different monogenic causes of high blood pressure are currently known. In several of these conditions, people who are affected also have measurable disturbances in the salt composition of the blood,” says Berge.
GWAS studies (genome-wide association studies), where gene variants in hundreds of thousands of people are compared in relation to the risk of a particular disease, have so far revealed more than 1500 genetic variants that have been found to be associated with altered blood pressure levels.
“Having a combination of several of these ‘unfortunate’ variants could explain why some people have higher blood pressure than others. It’s still too early to be able to apply this in a clinical context, but these findings could point to connections that are currently unknown. They increase our understanding, and in the long run the hope is that this will lead to more precise treatment,” says Berge.
Kidneys are in control
We find senior consultant Stein Hallan at the Division of Nephrology at St. Olav’s Hospital. He is also a professor in the renal medicine research group at NTNU’s Department of Clinical and Molecular Medicine and teaches in the medical study programme.
“High blood pressure is the domain of nephrologists,” Hallan says.
“The reason for that is that the kidneys are so important for managing blood pressure over time. Many things can raise blood pressure, but healthy kidneys are usually able to regulate the body so that the pressure remains normal. If you have something wrong with your kidneys, your blood pressure will also be problematic. And high blood pressure in turn damages the kidneys, so it becomes a repeating pattern.”
Hallan and NTNU are involved in several national projects where data from HUNT – the Health Survey in Trøndelag – is used to take a closer look at kidney damage and genetic changes in the kidneys in connection with high blood pressure.
“Almost all causes of hypertension are linked to the kidneys and the kidneys’ handling of salt,” says Hallan.
He says progress is being made in blood pressure research, although the search for the underlying causes is still ongoing.
“In most patients we don’t know the exact cause of the high blood pressure, but in some we can find a cause that can be treated. We find that some patients with hypertension produce too much of the hormone aldosterone.”
“This is a hormone that has to do with how salt is handled. The problem lies in the adrenal glands, where a benign tumour causes increased hormone production. Before we thought this condition was very rare, but now we’re finding more and more patients who have it,” says Hallan.
- You might also like: On the trail of a new medicine to treat multiple diseases
Goal is personalized treatment
Today, high blood pressure is treated with lifestyle changes and a combination of medications known to have a blood pressure-lowering effect. The doctors also rely on national and international drug recommendations that have a documented effect on morbidity and mortality in addition to their blood pressure-lowering effect.
At Oslo University Hospital, Berge believes that the aim should be to make use of genetic risk variants to identify people who have a high probability of developing high blood pressure.
“These individuals could then be tracked so that preventive drug treatment could start before organ damage occurs, and measures could be taken to reduce adverse lifestyle factors to an even greater extent.”
“And if you look even a little further into the future, the hope is to provide personalized treatment that is aimed specifically at the cause of an individual’s high blood pressure. Genetic analyses will also play an important role then,” says Berge.