Why you should be vaccinated even if you have had COVID-19
Even if you have had COVID-19, new vaccines will provide protection against new variants of the virus by helping the immune system produce antibodies.
“Vaccines help boost the production of antibodies, providing effective protection against serious illness and death,” says Mona Høysæter Fenstad.
Fenstad is a senior consultant at the blood bank at St. Olavs Hospital in Trondheim.
We are already well into autumn, and the COVID-19 virus is rife all over Norway. The Norwegian Institute of Public Health recommends people in risk groups to get vaccinated.
They point out that elderly people in particular will be vulnerable to serious illness if they are infected with COVID-19. However, since the vast majority of us have already had COVID-19 at least once, do we really need to think about getting vaccinated?
Yes, say the scientists.
“The saying ‘what doesn’t kill you makes you stronger’ is not true in this context. The inflammation that occurs in the body during infections such as influenza, COVID-19 and pneumonia can be harmful. Especially for people with heart or lung disease, or where other risk factors are involved,” says Fenstad.
Searching for medicine to combat COVID-19
Fenstand and her international colleagues have recently published a study that looked at the effect of vaccination on people who became ill with COVID-19 before vaccines were available. This work has been closely linked to the search for antibodies that can be used as medicine against COVID-19.
“At the beginning of 2020, the World Health Organization (WHO) asked scientists and therapists around the world to look for treatments for COVID-19. Among the treatments proposed was ‘convalescent plasma therapy’, which uses plasma from blood donors who have recovered from the illness. Along with NTNU colleagues, we chose to take a closer look at how the antibodies in this plasma were able to neutralize new virus variants that emerged,” says Fenstad.
While big pharmaceutical companies were working hard to develop vaccines and medicines, scientists had already begun to look at the use of blood plasma from COVID-19 patients as a possible treatment.
“Many of these patients had large amounts of antibodies in their blood. Plasma containing these antibodies was therefore given to seriously ill patients to help them fight the virus. It turned out that convalescent plasma therapy was primarily effective in patients who had immunodeficiencies,” says Fenstad.
A constantly changing virus
“We were looking for so-called ‘super-neutralizers’, people who develop specific antibodies that effectively neutralise different variants of SARS-CoV-2,” says Denis Kainov, a professor in NTNU’s Department of Clinical and Molecular Medicine who was part of the research team.
These antibodies were eventually cultivated and cloned, and then turned into medicines used to fight COVID-19.
In Norway, the first COVID-19 outbreak occurred in February 2020. The first Alpha variant was quickly followed by new, mutated variants named Beta and Delta. Omicron, which is currently the prevailing variant, was first reported in late 2021.
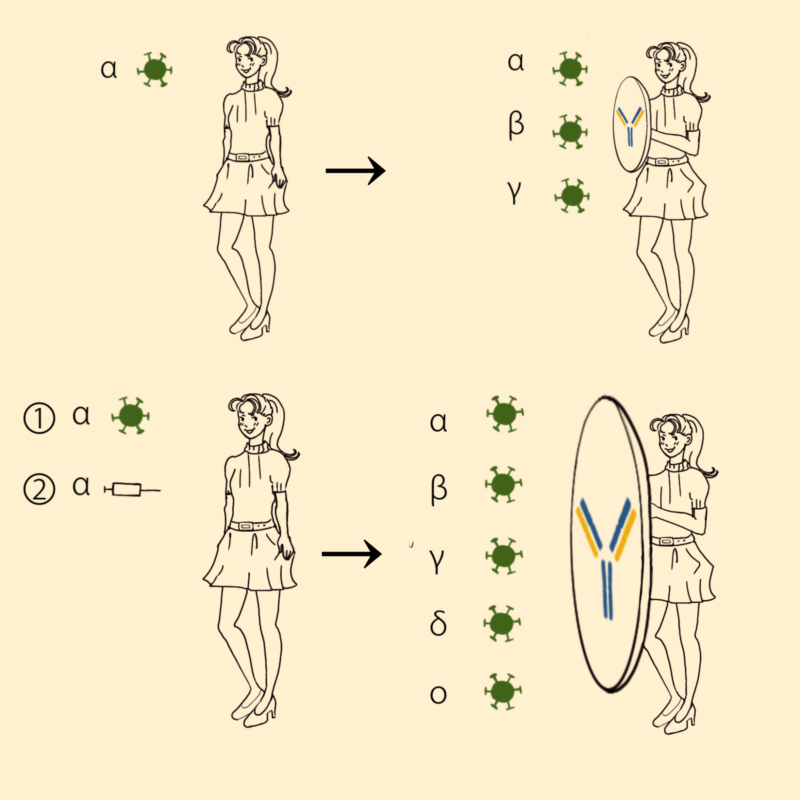
Top: A person is infected by the Alpha variant of SARS-CoV-2. Within a few weeks, antibodies are made that protect the person against the Alpha variant as well as Beta and Gamma variants which are very similar to the Alpha variant. Bottom: A person who (1) has recovered from COVID-19 and who (2) has received mRNA vaccine with components of the Alpha variant develops a strong immune response within a few weeks. The antibodies that are made in the body protect against the Alpha variant, the closely related Beta and Gamma variants as well as the more distantly related Delta and Omicron variants. People who have recovered from COVID-19 and then received the mRNA vaccine are also protected against new variants of SARS-CoV-2. Ill: Gerda Kaynova
By April 2020, blood banks across Norway had begun collecting blood plasma from patients who had recovered from COVID-19. At St. Olavs Hospital, 72 patients were selected for a more detailed study of the antibodies in their blood plasma.
“It turned out that half of these patients had serum containing antibodies that effectively neutralized the Beta variant,” says Kainov.
Found the dream patient
Kainov has been searching for active substances to use in the treatment of COVID-19 and other viral diseases.
He is now looking for antibodies that could provide wider protection, including against new COVID-19 variants that might emerge.
They noticed that four patients had antibodies that effectively neutralized the COVID-19 variant that was dominant in Trondheim at the time.
“We followed up by taking new samples from these patients and found that their antibodies also neutralized other COVID-19 variants. In fact, they were also effective on new virus variants,” says Kainov.
The conclusion is thus that it is a good idea to get vaccinated even if you have already had COVID-19 and even if the virus has mutated since the vaccine was made.
Out of the four patients, the scientists picked the one whose antibodies had been least effective against the Omicron variant. This patient had received their first vaccine dose four months after recovering from COVID-19. The efficacy of the vaccine was striking.
“The vaccine boosted the production of immune cells and antibodies against all tested variants of the virus, including Omicron,” says Kainov.
The virus is always one step ahead
Kainov’s colleagues in Estonia could then proceed with blood plasma from the patient, cloning and cultivating antibodies that neutralised COVID-19 viruses on a wide scale.
The results have also provided the scientists with useful knowledge about the effect of the vaccine on convalescents.
“When it comes to vaccines, it is always a race. The virus is always one step ahead, and the vaccines and medicines will never be completely up to date,” Fenstad said
“Our study is an in-depth study of just one patient, and it constitutes only a tiny piece of research in this field. However, large studies in other countries confirm our findings. Vaccines boost the production of antibodies that are also effective against new variants of the virus,” she said.
The finding demonstrate that it is a good idea to get vaccinated even if you have already had COVID-19 and even if the virus has mutated since the vaccine was made. It may not prevent you from being reinfected, but it will provide protection against serious illness and death.
“When you get sick with COVID-19, you develop antibodies, but the effects of these diminish and are gone after six to nine months. This is why people can get infected again and again by new variants of SARS-CoV-2. The virus mutates to avoid the immune response we have developed through previous infections or vaccines,” says Kainov.
That is why vaccination is important now that we are heading towards winter.
“The studies we have conducted here on COVID-19 patients are extremely important, because there will be new outbreaks of the virus. Almost seven million people have died from COVID-19. We must avoid getting into the same situation again,” says Kainov.
Reference: Mona Høysæter Fenstad et al.: Boosted production of antibodies that neutralized different SARS-CoV-2 variants in a COVID-19 convalescent following messenger RNA vaccination – a case study. International Journal of Infectious Diseases. Volum 137, December 2023
https://doi.org/10.1016/j.ijid.2023.10.011