A view into you
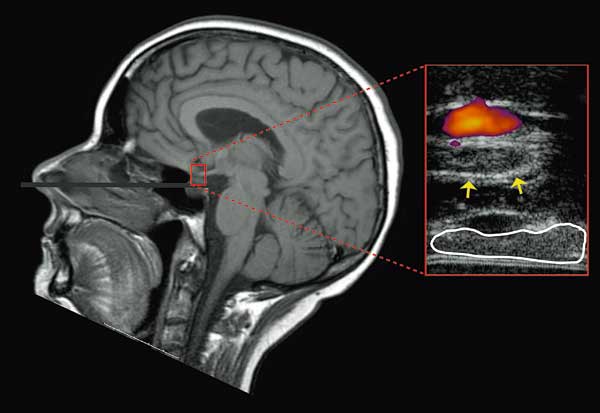
Ultrasonics improves a surgeon’s view in the removal of tumours from the pituitary gland.
Hidden in a little hollow in the skull, at about the level of the eye, we have a gland about the size of a black currant. This is the hypophysis, or pituitary, the body’s centre for hormone manufacture. The gland produces a wide range of hormones which in turn control other organs that manufacture yet more hormones.
Every year, some 120 Norwegian patients are operated on tumours in the pituitary gland. Now SINTEF, NTNU and St. Olavs Hospital in Trondheim have joined forces to develop an ultrasonic instrument that give Trondheim’s neurosurgeons an extra “eye” during interventions of this sort.
Promising method
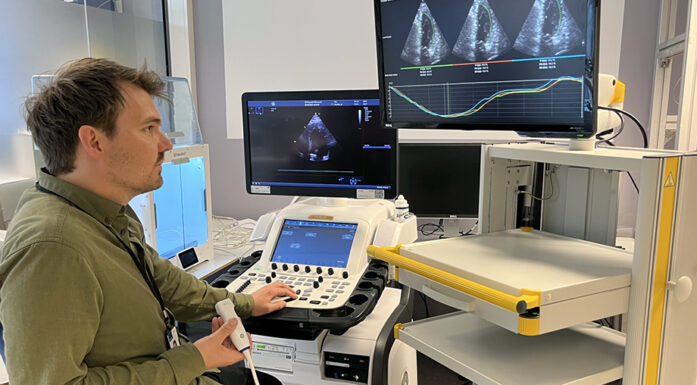
Assistant physician and doctoral candidate Ole Solheim describes the new operation aid as very promising.
“We are probably able to remove more tumour tissue than we would have been able to do otherwise, which reduces the chances of the tumour returning, and increases the likelihood of obtaining a nearly normal hormonal balance. The instrument also makes it easier to see where the tumour cells lie relative to the optic nerves and blood vessels – structures close to the pituitary that we must avoid damaging during the operation.”
For the moment, use of the new instrument has the status of experimental treatment. The new “window” on the inside of the skull has been used on 15 patients at St. Olavs Hospital.
In earlier days, people afflicted with pituitary tumours might well end up in circus freak shows, because the cocktail of compounds that are produced by the pituitary includes growth hormones.
Certain pituitary tumours may produce abnormal patterns of growth before the body is fully grown. If the illness develops later in life, it can result in a very heavy body shape, and in the worst cases, a lethal stress on the patient’s heart. Tumours may also cause pressure on other brain tissue and produce damage there.
More study needed
Solheim emphasizes that large-scale comparative studies of operations on pituitary tumour patients are needed before the value of the ultrasonic instrument can be documented. However, he points out that even the best aids can never guarantee that an operation will not lead to complications.
In the development of the instrument, SINTEF’s Tormod Selbekk, and Lasse Løvstakken and Tonni Johansen of NTNU were the main contributors on the technology side.
The 3D Ultrasound Centre of Expertise, the Research Council of Norway and the Central Norway Regional Health Authority have all helped to finance the development of the new surgical aid. SINTEF, NTNU and St. Olavs Hospital have joined forces with the Norwegian company Sonowand to continue the development of the instrument.
Svein Tønseth
Contact: Tormod Selbekk, SINTEF Technology and Society
Phone: +47 905 44 733 Email: Tormod.Selbekk@sintef.no