Big differences in how emergency doctors assess patient care needs
The threshold for admitting patients to the hospital varies greatly between emergency physicians. The doctors most willing to admit patients refer almost twice as many elderly patients as the most restrictive physicians.
In a recent NTNU study, researchers divided out-of-hours general practitioners (GPs) into four groups based on how often they admit their patients to the hospital. If you are seen by a doctor who belongs to the 25 per cent who admit the most often, your chance of a hospital stay is much greater.
Patients over the age of 69 have almost double the chance of being admitted to hospital by GPs with higher admission rates as compared with patients who see a GP in the lowest admission rate group.
One might reasonably believe that the patients who have seen the most restrictive out-of-hours (emergency) doctors will eventually have more hospital admissions down the road. To some extent this does happen.
However, 30 days after an emergency room visit, findings still show fewer admissions among the patients who were seen by the most restrictive GPs than among those whose physicians were most likely to send the patient to hospital.
One-third of all admissions
- Emergency rooms – or out-of-hours services – are run by the municipalities. Their purpose is to treat acute conditions outside the GPs' working hours.
- The emergency room has the authority to admit patients to hospitals.
- More than a third of all hospital admissions come from emergency rooms.
Expensive for hospitals
“This means that the GPs with the lowest threshold for admission inflict significant costs on the hospitals that might be unnecessary,” says PhD candidate Ellen Rabben Svedahl.
Doctors who admit patients the most often cost about NOK 4.2 million more per 1000 emergency room visits.
“Our study findings show that a GPs’ out-of-hours decision to admit a patient affects the total use of health services and hospital costs. We’ve calculated that the doctors who admit patients the most often cost about NOK 4.2 million more per 1000 emergency room visits than the GP group with the fewest referrals,” Svedahl said.
With approximately 200 000 emergency consultations a year for the over-69 age group, this becomes a major cost. Svedahl and her supervisor Johan Håkon Bjørngaard, a professor in the Department of Public Health and Nursing, are part of a group at NTNU that studies health services, funded by the Research Council of Norway.

An ageing population and higher life expectancy mean that the need for emergency care and specialist treatment will increase. Photo: Shutterstock, NTB
Risk of death not any higher
But doesn’t the risk to patients’ lives and health increase when they’re seen by doctors who have the highest threshold for admission?
We didn’t find that different admission thresholds lead to differences in patients’ 30-day risk of death.
Svedahl says the researchers didn’t find that different admission thresholds led to differences in patient mortality over the 30 days following the out-of-hours visit.
“At the same time, we know that too few – or too many – hospitalizations can potentially mean an increased risk of complications, especially for the elderly. What we didn’t investigate is how satisfied the patients were, or whether any complications arose in the long term,” Svedahl said.
Gender and age differences
The researchers grouped doctors according to their frequency of hospital admissions, independent of gender and age. But they also found that men and women, as well as younger and older doctors, have different practices. When children aged 0-10 years are seen by a female GP in the emergency room, the admission rate is 25 per cent higher than if the GP were a man.
The propensity to admit patients decreases by 5-8 per cent with every decade older that a physician is. Specialist-trained doctors are a little less likely to refer their patients to hospitals, while CPs with low out-of-hours experience in the previous two years tend to admit more.
Riskier to see a male doctor?
Gender and age differences have been found in previous studies, but little research has been done on the consequences of different thresholds for admission.
Is the risk to patient safety greater if you are examined by a male doctor or an older doctor?
“Although the doctor’s gender and age indicate some differences, they’re quite small and even out somewhat over time after the out-of-hours contact. The costs for the specialist health services thus aren’t that much lower, even though male and older doctors are more restrictive in referring patients to hospital,” says Svedahl.
Slightly higher mortality
The researchers found that mortality was slightly higher (12-17 per cent) among patients seen by doctors who had less emergency room practice during the previous two years.
We can’t ignore the fact that some patients are sent home who should have been hospitalized.
“Here we have to allow for some uncertainty. However, we can’t ignore the fact that some patients are sent home who should have been hospitalized. Another possible explanation is that older, more fragile people were admitted who shouldn’t have been sent to hospital. This should be further investigated,” Svedahl says.
One in four over the age of 70 admitted
- In the group of 0-10 year old children, 6.2 per cent were admitted to hospital within ten hours after the emergency room visit.
- For the age group 11-69 years, 12.4 per cent were admitted.
- For patients aged 70 and older, 25.8 per cent were admitted to hospital and 4.6 per cent died during the first 30 days.
Warns against raising the threshold
Does that mean that doctors should raise the threshold for hospitalization?”
A more restrictive hospital admissions practice could affect patient safety.
“The question is rather how we can ensure the quality of admissions in the best possible way. The study shows that a more restrictive hospitalization practice could affect patient safety,” says Svedahl.
In Norway, GPs are the largest group of physicians that rotate through emergency room shifts. Limited time and little knowledge of the patients means that out-of-hours doctors have a poorer basis for making their assessments than in their primary care practice as a GP.
Svedahl believes better systems – such as greater opportunities to confer with another doctor or specialist, introduction of shared patient records and more systematic feedback on how patients are doing after referral – could contribute to increasing the quality of care.
Admission in emergency care centres
Some municipalities have established out-of-hours emergency care centres where patients can be admitted.
The work pressure among GPs could weaken out-of-hours services.
“Schemes like this give the emergency doctor several options. Instead of admitting patients with questionable needs to hospitals or sending them home, they can be referred to a 24-hour unit in the out-of-hours primary care centres where they receive treatment, care and are observed by GPs and nurses,” says Svedahl.
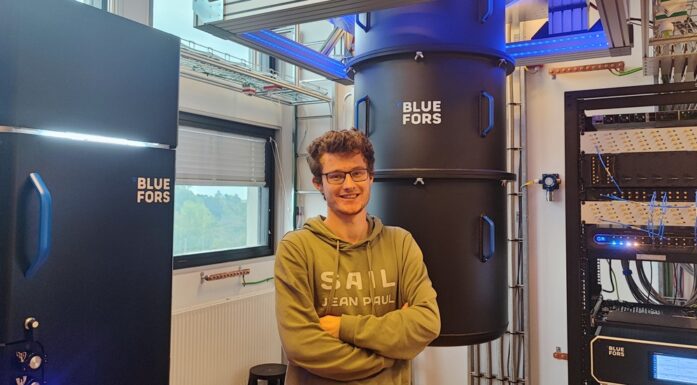
An ageing population and higher life expectancy mean that the need for emergency care and specialist treatment will increase. Svedahl, who is also a physician, is concerned that the work pressure among GPs could weaken out-of-hours services.
“Many GPs report high work pressure. This could mean that we’ll have fewer doctors with a lot of experience in out-of-hours emergency centres. This situation might in turn lead to more hospital admissions, higher costs and increased pressure on the specialist health services,” she says.
- You might also like: Hip fracture outcomes worse during busy periods
Study design
Studying hospitalization practices is difficult due to varying morbidity in the doctors’ patient groups.
“We were careful about how we made the comparisons. A patient in his 70s who saw a doctor in the emergency room on a Wednesday was only compared with other patients in their 70s who saw another doctor in the same emergency room on the other Wednesdays in the same month. This means that we only compared patients who saw other doctors in the same emergency room for comparable periods of time. With this design, we assumed that the differences we found would not be due to the different doctors having patients with varying morbidity,” Svedahl explains. The researchers used data from all emergency room visits in the period 2008-2016.
Seeing how services are linked
“The study is another example that points out the need for primary and specialist health services to be seen in a linked context,” says Professor Johan Håkon Bjørngaard.
“An intensified effort in out-of-hours emergency care is more expensive for the municipalities, but can be better for the patient. It can also reduce the pressure on the specialist health services and would be a good use of resources for society,” he said.
Reference: Ellen Rabben Svedahl et al.: Effects of GP characteristics on unplanned hospital admissions and patient safety. A 9-year follow-up of all Norwegian out-of-hours contacts, Family Practice.