50,000 Norwegians require more morphine than the average Joe
When one patient received 60 times the normal dose of morphine, and still didn’t notice anything, the doctor called NTNU. Now researchers know why this patient didn’t respond to the pain medication.
PAIN MANAGEMENT: For the first time, researchers have documented that about one in every hundred Norwegians needs a double dose of pain medication to get the same effect as other people. About 50,000 people need a significantly higher dose than normal. And about a hundred people in Norway are completely resistant to opioids such as morphine.
Significant for cancer patients
The findings are of great importance for patients when they are operated on, or for individuals who are in severe pain – such as cancer patients.
A few years ago, Pål Klepstad, a professor at NTNU and an anaesthesiologist at St. Olav’s Hospital in Trondheim, received a call from a physician colleague in western Norway. What started out as a routine operation subsequently turned out to solve a riddle among doctors and researchers:
Why do some patients require much higher doses of pain medication than others?
- You might also like: Living longer, but with illness and pain
Doctor kept increasing the dose – with no effect
The patient, who was to be operated on for a hernia, had received the standard dose of a powerful painkiller, remifentanil, but it had no effect. So the doctor increased the dose. And increased it again. And again. Eventually, the patient had received 60 times the usual dose. But still he felt no effect. The doctor was amazed and called Klepstad in Trondheim.
Klepstad contacted fellow professor Frank Skorpen at NTNU’s Department of Laboratory Medicine, Children’s and Women’s Health. Together they decided to investigate. They obtained permission from the patient to examine his genes via a blood test. Skorpen first tested for the most common genetic variants that might be suspected of influencing how pain medications work, but found no clues as to why the drug had no effect.
Special gene mutations
Enter NTNU PhD candidate Anne Heidi Skogholt, who was researching the gene that determines how opioids bind to the brain. When the researchers then analysed the patient’s blood sample more extensively, they understood why the patient didn’t react to 60 times the normal dose of morphine. The patient had a special gene mutation, which had been described in the literature only once before – in a person in the United States.
What does it mean to have a gene defect like this?
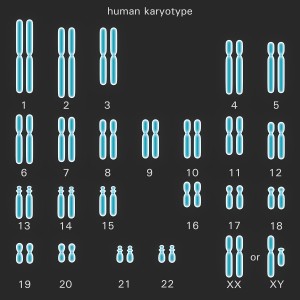
We all have 46 chromosomes, arranged in 23 pairs. We inherit one chromosome set from each of our parents. Two of these chromosomes, X and Y, determine our sex. The patient who was resistant to morphine had the same mutation on both chromosomes in the same pair. The error causes the body’s normal response to opioid pain killers, such as remifentanil, morphine, methadone and fentanyl, not to work. The opioids bind normally in the brain, but the signal isn’t sent on to stop the pain.
This triggered Skorpen’s curiosity: how many people in the Norwegian population might have this genetic error?
Could be suspected of using drugs
Skorpen obtained permission to check 600 healthy blood donors at St. Olav’s Hospital, whose data Professor Ola Dale had collected as part of a related research project. Skorpen was able to document that approximately one person out of a hundred had this genetic defect on one chromosome in one pair. This means that these people would probably need a double dose of opioid pain medication to achieve the same effect as people without this error. Skorpen and Klepstad further examined over 2,000 cancer patients, and calculated that one person in 40,000 will have this hereditary syndrome on both chromosomes in the same pair. These are the individuals who are completely insensitive to opioids.
“Many of the patients who need a double dose could easily be misunderstood by doctors. They might try to alter their prescriptions to get the effect they need, and be suspected of wanting to get high. It’s important to emphasize that some patients actually need more painkillers to get the help they need,” says Klepstad.
- You might also like: The pain paradox
Totally different treatment
For patients who are resistant to opioids, doctors need to adjust the treatment, whether the patient is undergoing surgery or has intense pain due to cancer. One solution may be an epidural pump or anaesthesia.
“It’s a simple matter to test whether someone has this genetic defect that leads to reduced efficacy or insensitivity to opioids,” says Skorpen.
“But this is new information, and this test isn’t routinely run in hospitals,” Klepstad adds.
The body’s natural pain relief
Thirty per cent of people in Norway report that they live with chronic pain. Skorpen and Klepstad now want to investigate whether there may be more people with this genetic defect among those who suffer from chronic pain. The gene error may also mean that the body’s natural system for pain relief is not up to snuff, either. Skorpen and Klepstad will start their investigation with data from Norway’s longitudinal HUNT study.
For the record: The patient who received 60 times the normal dose of remifentanil was not harmed by it. When the body does not respond to the drug, nothing happens, and the body excretes this medication relatively quickly.